Template File: /www/wp-content/themes/stn2017/single.php | Template Hierarchy
WP version: 6.5.5
PHP version 8.2.21
The development of the Major Trauma Service in the West of Scotland came with significant resource to provide rehabilitation in order to achieve the Scottish Trauma Networks stated aim of: Saving Lives. Giving Life Back.
The rehabilitation team within the Major Trauma ward in the Queen Elizabeth University Hospital are delivering early, intensive, multidisciplinary rehabilitation to patients who are multiply injured and have complex rehabilitation needs. The team consists of speech and language therapists, physiotherapists, occupational therapists, clinical psychologists, dietitians, therapy support workers and major trauma co-ordinators.
Initial results are extremely positive and a number of QI projects have also been carried out. An analysis of the data collated since the Major Trauma ward opened in August 2021 shows that the median length of stay in the ward is 10 days. It also showed that 69.4% of patients were discharged straight home from the ward and 20.6% required repatriation to their local hospital. This has contributed to an improved patient journey and in these times of significant pressure on the NHS, is reducing the requirement for ambulance transfers and beds in trauma units.
“a set of measures that assist individuals, who experience or are likely to experience disability, to achieve and maintain optimum functioning in interaction with their environments”
(WHO, 2011)
Evidence shows that the earlier rehabilitation is provided and the greater the intensity, the better the outcomes for the patient (Hartley, Keevil, Alushi et al, 2019). It was with this evidence in mind that the ethos of the STN was developed.
The rehabilitation needs of medical inpatients is changing. Development of community based, admission avoidance schemes means that patients admitted to hospital tend to be more unwell and have more complex rehabilitation needs. This has been exacerbated by the COVID-19 pandemic: patients are more frail, deconditioned, present later in disease course and a significant proportion have underlying neurological diagnosis.
Ongoing challenges around bed capacity and ‘front door’ performance forced the opening of additional medical beds in the QEUH in October 2021. The current staffing complement within the medical sector is not able to meet the rehabilitation needs of the patients (Staff to patient ratios: Physiotherapy (PT) = 1:41, Occupational therapy (OT) = 1:56). This means that patients who are assessed as requiring rehabilitation, are seen on average twice a week.
Current staffing resource within the AHP team does not meet the rehabilitation needs of the patients who are located within medical, resulting in longer lengths of stay and reduced independence on discharge requiring significant packages of care and equipment provision. This has financial implications for the NHS in terms of bed days and equipment provision, and for Social Care in terms of ongoing provision of support at home, in addition to the detrimental effects for patients who they are not being facilitated to achieve their maximal functional potential.
Ward 11D was turned fully into a medical ward in October 2021. As no additional AHP staff were provided for these additional bed numbers, and with medical AHP staffing numbers already being low, the AHP Team from the Major Trauma ward were asked to cover these additional medical beds.
This situation was used as an opportunity to collect data on what therapy input and therapy resource was required by the patients within this area to ensure the best quality of care was provided to patient and service and assess the impact of enhanced staffing levels on patient length of stay and outcome.
PT and OT staff from the Major Trauma ward team were assigned to cover the additional medical beds, these staff had experience in neurorehabilitation and were a mix of bands from 6 to 8B.
Increased staff to patient ratio was made available compared to ‘normal’ staffing levels on established general medical wards.
All patients referred to PT/OT over a 6 week period were included.
Patients were provided with daily therapy input as required.
Rehabilitation need and complexity were quantified using the standardised Rehabilitation Complexity Scale (RCS-E)
Data on number of referrals, diagnosis, reason for admission, number of treatment sessions, hours of treatment and number of therapists required for each treatment session was collected in addition to length of stay, and requirement for onward referral to community teams or for packages of care at point of discharge.
Data was collected from both the intervention ward (with enhanced AHP staffing levels) and a comparator ward (with ‘normal’ medical AHP staffing).
The data gathered from both areas is summarised in the following table:
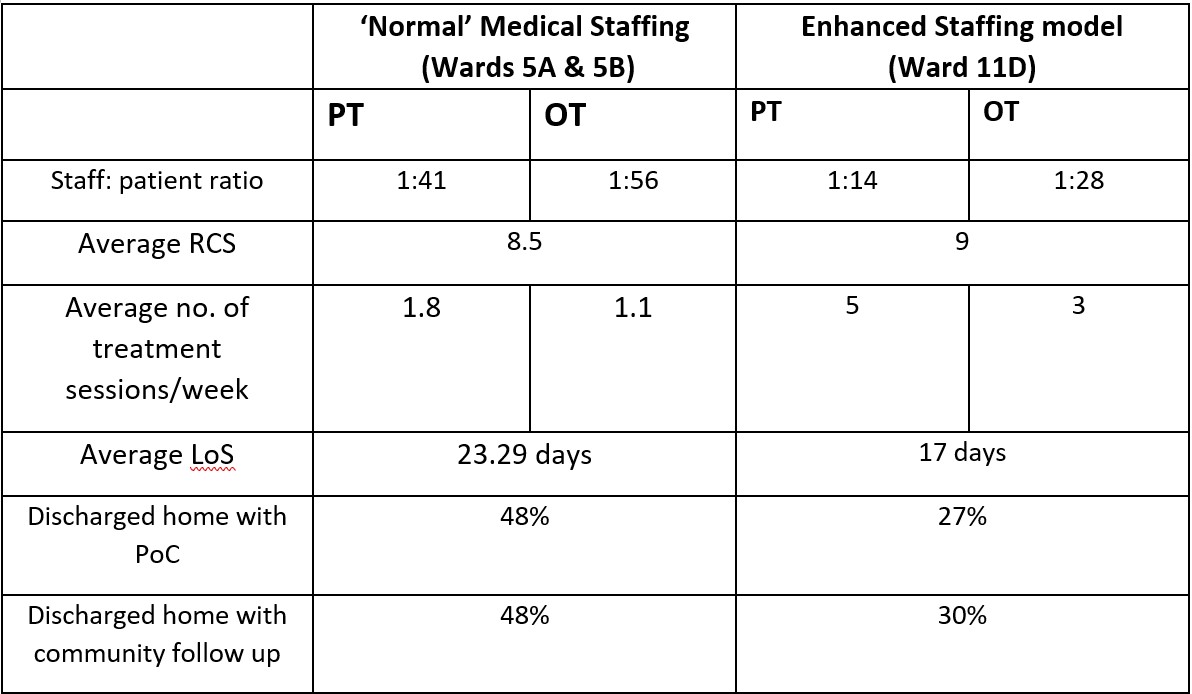
Specific case studies and anecdotal evidence from the Major Trauma team’s time covering 11D showed that it was not only the number of staff available to treat patients that had a positive impact on LOS and patient outcomes. They also found that having staff who were knowledgeable and had experience treating patients with neurological diagnosis with complex rehabilitation needs, was beneficial.
The data highlights that the right number of staff and experience has a significant impact on reducing patients LOS and improving patient outcomes. In this audit LOS was reduced by 6.29days and less patients were referred onto community rehabilitation teams therefore suggesting they achieved their rehabilitation potential in hospital as they received the right amount of specialist treatment. Additionally, significantly fewer packages of care were required for the patients discharged home. This evidence suggests that early and adequate provision of OT/PT intervention is beneficial not only for patients but also for the hospital.
Overall, the data gathered supports the conclusion that improved PT and OT staffing levels can have a positive impact on length of stay and patient outcomes for patients with complex rehabilitation needs, currently managed within medical wards. Ultimately this could result in reduced spend on bed days, equipment provision and care needs for these patients.
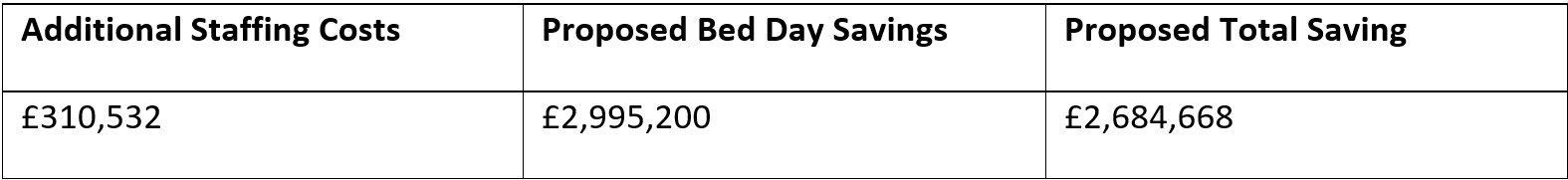
The planning and finance department calculated that based on the proposed figure of 416 patients being discharged each year, with an average reduction in length of stay of 6 days per patient, this could potentially save 2496 bed days per year. Based on a cost of £1,200 per day for a general medical bed, this would equate to a saving of £2,995,200 for bed days.
Implementation of the Major Trauma service in the West of Scotland came with significant allocation of resource for rehabilitation. This is to provide early, intensive rehabilitation in line with the British Society for Rehabilitation Guidelines (BSRM, 2015) in order to meet the networks aim of ‘Giving Life Back’.
There is a growing body of evidence which links at least daily multidisciplinary rehabilitation provision with an improvement in long term functional ability (Fan et al, 2020), particularly in patients following acquired brain injury (Konigs et al, 2018).
For patients not on the Major Trauma pathway, this level of daily intervention is not possible due to limited AHP and clinical/neuropsychology rehabilitation resource within the acute neurosurgical service at the Institute of Neurological Sciences (INS). The project compares the rehab provision in INS to major trauma who are staffed at an appropriate level.
Aims
Six patients with a diagnosis of brain injury who did not follow the MT pathway were identified and compared with six patients with similar demographics and initial presentation who followed the MT pathway.
Patients were highlighted for the comparison project by the Head Injury Advanced Practitioners at the QEUH.
Outcome measures used: Rehabilitation Complexity Scale (RCS) and the Functional Independence Measure + Functional Assessment Measure (FIM+FAM).
Data was collected on length of stay, disciplines involved, therapy attendances/hours and discharge destination.
Although a small sample size it highlights the variation for patients with similar presentations.
Outcome measures: Improvement in both outcome measures with average FIM+FAM score increasing (by 94 compared to 49) and RCS score decreasing (-9 compared to -5) for MT patients.
In addition to the significantly better patient outcomes on the major trauma pathway it also highlights:
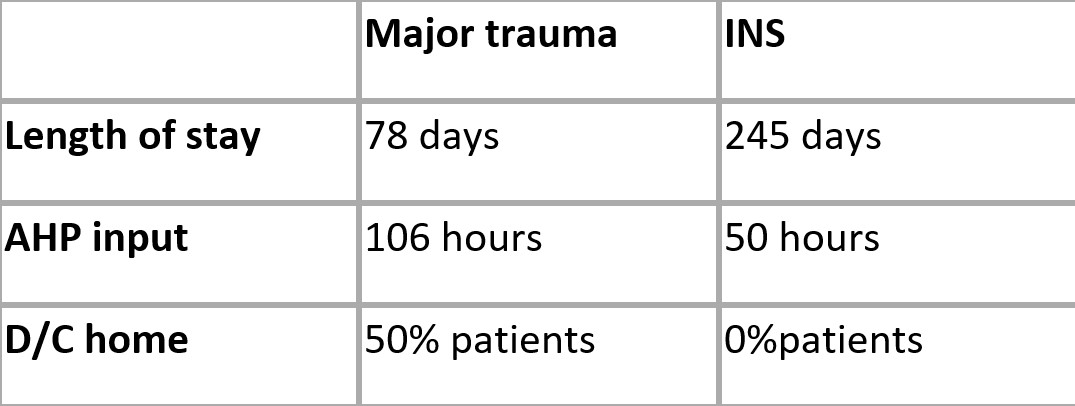
The results of preliminary examination appear to support the hypothesis that patients following the MT pathway, who receive early, intensive, daily input from a multidisciplinary team, have a reduced length of stay and improved functional outcomes compared with those who are not on the MT pathway.
Ongoing research in conjunction with INS colleagues is indicated to yield a larger sample size and determine the reliability of these results and the associated cost savings in relation to bed days in an inpatient bed and long term care needs.
In addition to the findings from the two pilot projects completed, an analysis of the data collated since the Major Trauma ward opened in August 2021 shows that the median length of stay in the ward is 10 days.
It also showed that 69.4% of patients were discharged straight home from the ward and 20.6% required repatriation to their local hospital. This has contributed to an improved patient journey and in these times of significant pressure on the NHS, is reducing the requirement for ambulance transfers and beds in trauma units.
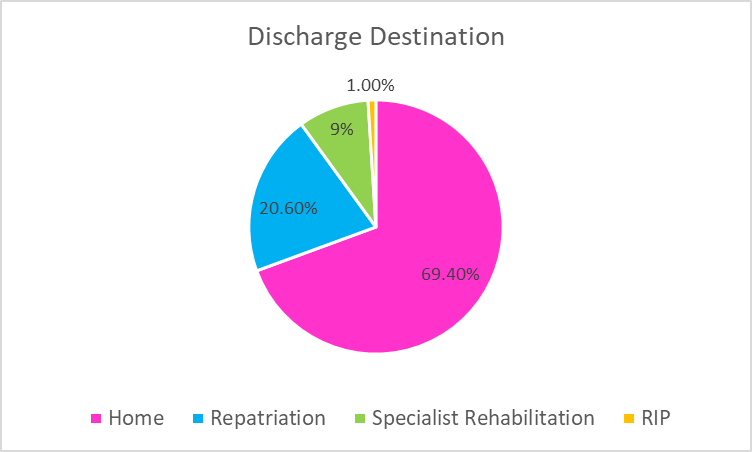
Of the patients that were discharged home, only 24% of them required onward referral for community follow up (Community Rehab Teams, MSK services, Brain injury Teams). Additionally only 6% of patients required a Package of Care at point of discharge.
These results are further evidence that having adequate rehabilitation resource which allows early, specialist multi-disciplinary rehabilitation to be carried out result in shorter length of stay, improved patient flow, improved patient outcomes and a reduction in the requirement for packages of care and community rehabilitation on discharge. The provision of this resource is therefore a benefit to both major trauma patients and the service.