Template File: /www/wp-content/themes/stn2017/index.php | Template Hierarchy
WP version: 6.5.5
PHP version 8.2.21
The West of Scotland Paediatric team recently held their first Paediatric Major Trauma Study Day at the Major Trauma Centre in Glasgow.
The aim was to increase knowledge of the Scottish Trauma Network, and the services available at a Major Trauma Centre. Topics covered at the event ranged from Paediatric pelvic injuries and trauma imaging to outcome measures for brain injuries. Speakers included prehospital staff, consultant specialist surgeons and AHP staff to represent how Paediatric patients are treated and managed within a Major Trauma Centre from the front door, though their rehabilitation and discharge.
The event was available to staff both in person and online via Microsoft Teams, which proved popular with over 170 people attending the event. The importance of optional virtual attendance was highlighted with 70% of staff attending virtually. The event had attendees from across the West of Scotland Trauma, as well as staff from across Scotland, England, Wales and Northern Ireland.
Feedback received from attendees was extremely positive, with an average overall rating of 9 out of 10. Attendees praised the variety of the content and range of speakers across the entire Multi-Disciplinary Team within the trauma setting, as well as the remarkably patient story.
“Hearing the patient story and the recognition of the work of the Rehab team and MT Coordinators”
“Loved all of the different speakers and realising that it really is a multidisciplinary team effort and not just one individual”
The day proved so popular that the Team have planned to make this an annual event. They would like to once again thank all attendees, speakers and those who helped to support the day.

Chelsey Smith was 15 when she was left with life-threatening injuries, following a road traffic accident in February last year.
After an initial assessment at the University Hospital in Wishaw, Lanarkshire, Chelsey was rushed to the West of Scotland’s Paediatric Major Trauma Centre in Glasgow for specialist treatment.
Consultant Paediatric Neurosurgeon Roddy O’Kane performed the surgery, to reduce the swelling and pressure on Chelsey’s brain, with part of her skull being removed and stored in her stomach to keep it sterile.
Following intensive rehab with the team at the RHC, Chelsey, who is now 16, has made a remarkable recovery and, less than a year after her final surgery, was a guest of honour at the Major Trauma Centre’s training day this week.
She said: “I just can’t thank all of the team here at the Royal Hospital for Children in Glasgow for everything they have done for me, they have saved my life and given me my life back too.
“I don’t remember much about the day of the accident to be honest, but I’m here now and that’s what matters. I have had so much support from Roddy, my Major Trauma Co-ordinator Lynsay Stewart, all of the staff at the hospital and of course my family.
“Roddy was able to magically take a part of my skull and put it in my stomach to let the swelling reduce in my brain, I don’t really know how it works but it’s amazing. It was a long journey and I would tell anyone who is in a similar situation to keep going, to make this recovery you have to be mentally prepared for it too and thankfully I had so many positive people around me to help with that.”
Chelsey is now back preparing for her exams at Brannock High in Newarthill, has been able to get a part-time job and is hoping to go on to study accountancy.
She said: “Obviously everything that happened was not good, but thanks to the Royal Hospital for Children team in Glasgow I have been able to get back to school and have also started a part-time job.
“I just want to say thank you again to everyone for all they have done for me. Even after my follow-up appointments are finished, I’ll keep coming back to visit, I have missed them all.”
The procedure which involves removing part of the skull is not common, but after other medical interventions were unsuccessful it was the last option to save Chelsey’s life.
Roddy said: “This procedure is not something that we do every day but it gave Chelsey the best chance of surviving the injuries she had sustained during the accident.
“We take part of the skull out and store it in the stomach in order to keep it sterile, this is usually re-attached after a couple of months once swelling has reduced.
“Chelsey’s recovery is absolutely remarkable, based on her condition when she arrived it is incredible to see how well she is doing. There was a real danger to her life and we also anticipated that there would be more of lasting impact on her life.
“We are all so proud of Chelsey and all of the hard work she has put in during her rehab with our specialist teams. We’re delighted for her and her family and were all beaming from ear to ear when we got to see her again today.”
The development of the Major Trauma Service in the West of Scotland came with significant resource to provide rehabilitation in order to achieve the Scottish Trauma Networks stated aim of: Saving Lives. Giving Life Back.
The rehabilitation team within the Major Trauma ward in the Queen Elizabeth University Hospital are delivering early, intensive, multidisciplinary rehabilitation to patients who are multiply injured and have complex rehabilitation needs. The team consists of speech and language therapists, physiotherapists, occupational therapists, clinical psychologists, dietitians, therapy support workers and major trauma co-ordinators.
Initial results are extremely positive and a number of QI projects have also been carried out. An analysis of the data collated since the Major Trauma ward opened in August 2021 shows that the median length of stay in the ward is 10 days. It also showed that 69.4% of patients were discharged straight home from the ward and 20.6% required repatriation to their local hospital. This has contributed to an improved patient journey and in these times of significant pressure on the NHS, is reducing the requirement for ambulance transfers and beds in trauma units.
“a set of measures that assist individuals, who experience or are likely to experience disability, to achieve and maintain optimum functioning in interaction with their environments”
(WHO, 2011)
Evidence shows that the earlier rehabilitation is provided and the greater the intensity, the better the outcomes for the patient (Hartley, Keevil, Alushi et al, 2019). It was with this evidence in mind that the ethos of the STN was developed.
The rehabilitation needs of medical inpatients is changing. Development of community based, admission avoidance schemes means that patients admitted to hospital tend to be more unwell and have more complex rehabilitation needs. This has been exacerbated by the COVID-19 pandemic: patients are more frail, deconditioned, present later in disease course and a significant proportion have underlying neurological diagnosis.
Ongoing challenges around bed capacity and ‘front door’ performance forced the opening of additional medical beds in the QEUH in October 2021. The current staffing complement within the medical sector is not able to meet the rehabilitation needs of the patients (Staff to patient ratios: Physiotherapy (PT) = 1:41, Occupational therapy (OT) = 1:56). This means that patients who are assessed as requiring rehabilitation, are seen on average twice a week.
Current staffing resource within the AHP team does not meet the rehabilitation needs of the patients who are located within medical, resulting in longer lengths of stay and reduced independence on discharge requiring significant packages of care and equipment provision. This has financial implications for the NHS in terms of bed days and equipment provision, and for Social Care in terms of ongoing provision of support at home, in addition to the detrimental effects for patients who they are not being facilitated to achieve their maximal functional potential.
Ward 11D was turned fully into a medical ward in October 2021. As no additional AHP staff were provided for these additional bed numbers, and with medical AHP staffing numbers already being low, the AHP Team from the Major Trauma ward were asked to cover these additional medical beds.
This situation was used as an opportunity to collect data on what therapy input and therapy resource was required by the patients within this area to ensure the best quality of care was provided to patient and service and assess the impact of enhanced staffing levels on patient length of stay and outcome.
PT and OT staff from the Major Trauma ward team were assigned to cover the additional medical beds, these staff had experience in neurorehabilitation and were a mix of bands from 6 to 8B.
Increased staff to patient ratio was made available compared to ‘normal’ staffing levels on established general medical wards.
All patients referred to PT/OT over a 6 week period were included.
Patients were provided with daily therapy input as required.
Rehabilitation need and complexity were quantified using the standardised Rehabilitation Complexity Scale (RCS-E)
Data on number of referrals, diagnosis, reason for admission, number of treatment sessions, hours of treatment and number of therapists required for each treatment session was collected in addition to length of stay, and requirement for onward referral to community teams or for packages of care at point of discharge.
Data was collected from both the intervention ward (with enhanced AHP staffing levels) and a comparator ward (with ‘normal’ medical AHP staffing).
The data gathered from both areas is summarised in the following table:
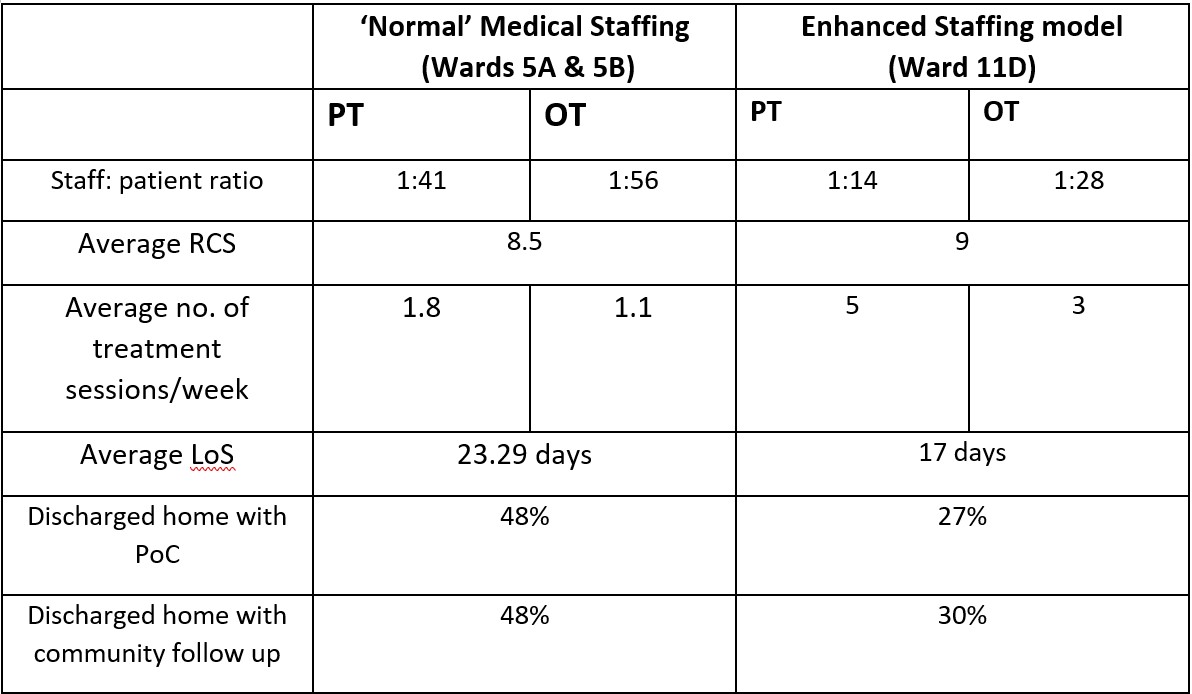
Specific case studies and anecdotal evidence from the Major Trauma team’s time covering 11D showed that it was not only the number of staff available to treat patients that had a positive impact on LOS and patient outcomes. They also found that having staff who were knowledgeable and had experience treating patients with neurological diagnosis with complex rehabilitation needs, was beneficial.
The data highlights that the right number of staff and experience has a significant impact on reducing patients LOS and improving patient outcomes. In this audit LOS was reduced by 6.29days and less patients were referred onto community rehabilitation teams therefore suggesting they achieved their rehabilitation potential in hospital as they received the right amount of specialist treatment. Additionally, significantly fewer packages of care were required for the patients discharged home. This evidence suggests that early and adequate provision of OT/PT intervention is beneficial not only for patients but also for the hospital.
Overall, the data gathered supports the conclusion that improved PT and OT staffing levels can have a positive impact on length of stay and patient outcomes for patients with complex rehabilitation needs, currently managed within medical wards. Ultimately this could result in reduced spend on bed days, equipment provision and care needs for these patients.
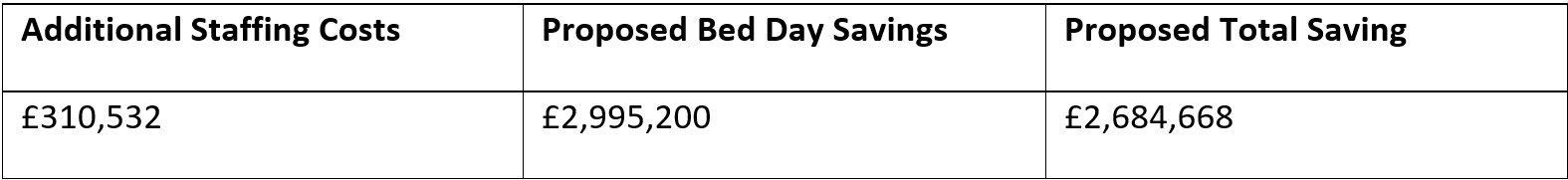
The planning and finance department calculated that based on the proposed figure of 416 patients being discharged each year, with an average reduction in length of stay of 6 days per patient, this could potentially save 2496 bed days per year. Based on a cost of £1,200 per day for a general medical bed, this would equate to a saving of £2,995,200 for bed days.
Implementation of the Major Trauma service in the West of Scotland came with significant allocation of resource for rehabilitation. This is to provide early, intensive rehabilitation in line with the British Society for Rehabilitation Guidelines (BSRM, 2015) in order to meet the networks aim of ‘Giving Life Back’.
There is a growing body of evidence which links at least daily multidisciplinary rehabilitation provision with an improvement in long term functional ability (Fan et al, 2020), particularly in patients following acquired brain injury (Konigs et al, 2018).
For patients not on the Major Trauma pathway, this level of daily intervention is not possible due to limited AHP and clinical/neuropsychology rehabilitation resource within the acute neurosurgical service at the Institute of Neurological Sciences (INS). The project compares the rehab provision in INS to major trauma who are staffed at an appropriate level.
Aims
Six patients with a diagnosis of brain injury who did not follow the MT pathway were identified and compared with six patients with similar demographics and initial presentation who followed the MT pathway.
Patients were highlighted for the comparison project by the Head Injury Advanced Practitioners at the QEUH.
Outcome measures used: Rehabilitation Complexity Scale (RCS) and the Functional Independence Measure + Functional Assessment Measure (FIM+FAM).
Data was collected on length of stay, disciplines involved, therapy attendances/hours and discharge destination.
Although a small sample size it highlights the variation for patients with similar presentations.
Outcome measures: Improvement in both outcome measures with average FIM+FAM score increasing (by 94 compared to 49) and RCS score decreasing (-9 compared to -5) for MT patients.
In addition to the significantly better patient outcomes on the major trauma pathway it also highlights:
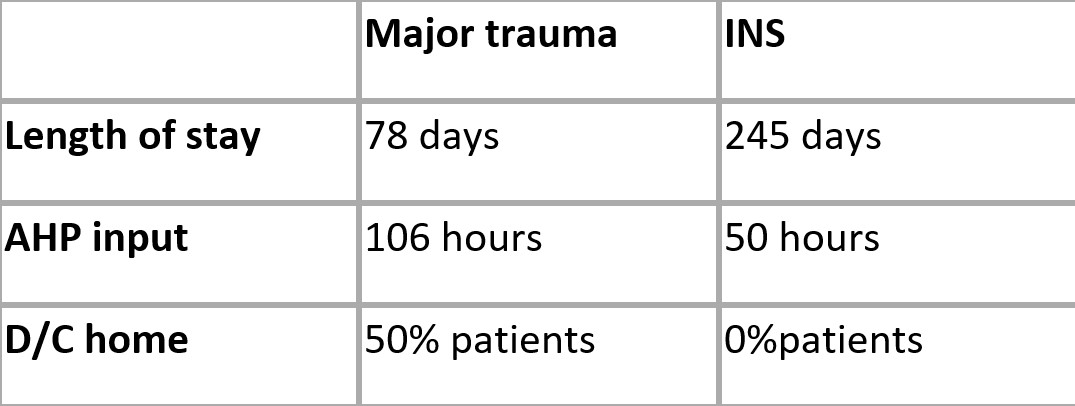
The results of preliminary examination appear to support the hypothesis that patients following the MT pathway, who receive early, intensive, daily input from a multidisciplinary team, have a reduced length of stay and improved functional outcomes compared with those who are not on the MT pathway.
Ongoing research in conjunction with INS colleagues is indicated to yield a larger sample size and determine the reliability of these results and the associated cost savings in relation to bed days in an inpatient bed and long term care needs.
In addition to the findings from the two pilot projects completed, an analysis of the data collated since the Major Trauma ward opened in August 2021 shows that the median length of stay in the ward is 10 days.
It also showed that 69.4% of patients were discharged straight home from the ward and 20.6% required repatriation to their local hospital. This has contributed to an improved patient journey and in these times of significant pressure on the NHS, is reducing the requirement for ambulance transfers and beds in trauma units.
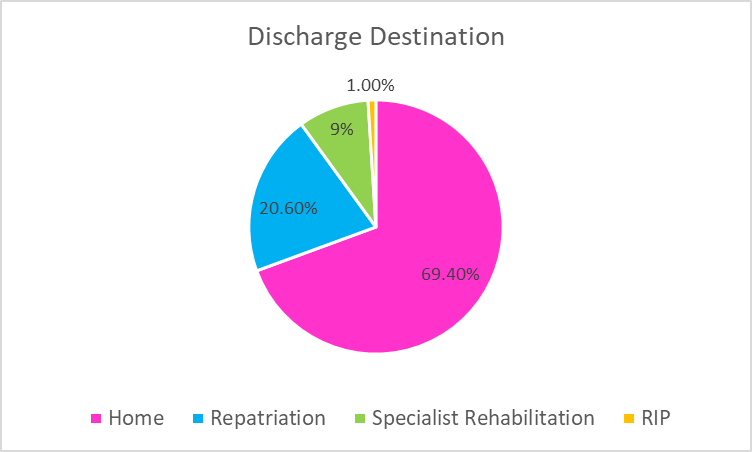
Of the patients that were discharged home, only 24% of them required onward referral for community follow up (Community Rehab Teams, MSK services, Brain injury Teams). Additionally only 6% of patients required a Package of Care at point of discharge.
These results are further evidence that having adequate rehabilitation resource which allows early, specialist multi-disciplinary rehabilitation to be carried out result in shorter length of stay, improved patient flow, improved patient outcomes and a reduction in the requirement for packages of care and community rehabilitation on discharge. The provision of this resource is therefore a benefit to both major trauma patients and the service.
The Scottish Trauma Network (STN) are pleased to announce the publication of the Nursing, Midwifery and Allied Health Professions (NMAHP) NMAHP Development Framework for Major Trauma.
This is hosted within the Education and Training section of the STN website;
https://www.scottishtraumanetwork.com/our-work/education-learning/
The NMAHP Development Framework for Major Trauma will be used by NMAHP practitioners caring for major trauma patients in any in-hospital setting at local, regional and national levels for identifying, planning and supporting learning needs, identifying career pathways and enhancing workforce planning.
This framework is the result of collaborative working between NHS Education for Scotland (NES) and the STN, working closely with NMAHP practitioners and consulting with the STN Education and Workforce group. It is aligned to the already published NES NMAHP Development Framework.
It is currently for registered practitioners at education levels 5-8 with the Healthcare Support Worker element following later in the year, in conjunction with the national HCSW commission.
Introduction by National Clinical Lead
Annual report time arrives once again, and in this new style of presentation my superlatives for the work of all who support the continued work, development and improvements of the Scottish Trauma Network will be brief. This is just as well, as the resources of my thesaurus begin to abate.
It is now 5 years since we convened and commenced our program of work to build and implement an entirely new clinical network of acute care and long-term rehabilitation for Scotland’s most seriously injured. August 30th 2021 witnessed the completion of Phase I with delivery of the fully operational end product. At time of writing, we run smoothly and successfully in the best traditions of “National Collaborative Pragmatism”.
All of this achieved of course, against the backdrop of complications presented to us by the pandemic. A remarkable achievement now recognised and acclaimed at the highest levels of the NHS, the Scottish Government, and national and international media.
This hard-earned and well-deserved reputation requires stiffening of the sinews and strengthening of resolve to be maintained, for us to progress further as we contribute well beyond our remit to the Remobilisation of the NHS in Scotland.
Thus, now begins Phase II, where we plan to tell the story using data, to raise standards for the future, and to demonstrate the sustained improved outcomes for patients, their families, their communities and the nation as a return on the visionary investment of these past 5 years.
The full report can be seen here
Martin McKechnie
National Clinical Lead
Scottish Trauma Network
The eighth report by the Scottish Trauma Audit Group (STAG) since 2011 can be found on the Public Health Scotland website. Compliance with a subset of the Scottish Trauma Network Key Performance Indicators, case-mix adjusted mortality and Patient Reported Outcome Measures (PROMs) are within part one of the report. Part two and three provide a comprehensive summary of injuries and the patient journey for both adults and paediatrics respectively.
Introduction from National Clinical Lead
2020 – 21 has been variously difficult, challenging, interesting and rewarding across the many spheres of activity, development and progress for the Scottish Trauma Network (STN). This Annual Report sits alongside and complements the imminent publication of the Scottish Trauma Audit Group’s (STAG) Annual Report for the same period. They both reveal and explore much of the data, operational and patient-centred clinical stories around this past year’s extraordinary activity within the Network. Set against the pandemic backdrop, the strong message coming from these reports is one of resilience, maintained high-quality patient care and an above-and-beyond spirit of collaboration and pragmatism on a national scale. That key performance and outcome measures have been delivered, yet alone maintained and improved in several areas, is worthy of acknowledgment and appreciation. The reports further explore much of our presentation and discussion at the Scottish Parliament Health and Sport Select Committee in January 2021.
There are many examples to celebrate, but I take this opportunity to highlight and express admiration and gratitude to the Scottish Ambulance Service, the ScotSTAR and EMRS transport and retrieval arms, and the newer Advanced Paramedics in Critical Care red teams therein. Their relentless and complex work in supporting and enabling the pandemic response across trauma and all related critical care services has been inspiring. The STN and patients are thankful to them beyond words. These thanks are expressed in equal measure to all staff and services recruited in good faith and optimism to the STN, yet who found themselves redeployed and reallocated to support the response in other vital areas such as Emergency Departments, Trauma Wards which became Covid High Dependency Units and Critical Care areas, and Theatres.
More interesting still is what much of this tells us about the improved access we now have to data and patient-reported measures. These are the mainstays of why the STN does what it does. With STN Trauma and STAG coordinators now embedded in our hospitals, we are able to reach more broadly across and deeper into the care of trauma patients than ever before. The resulting information and its analysis will further “tell the story” as we move beyond delivery of Phase I later this year, with the opening of the Major Trauma Centres at the Queen Elizabeth University Hospital in Glasgow, and the Royal Infirmary of Edinburgh, and the operational delivery of the Regional Networks in the West and South East of Scotland. These final pieces of the jigsaw will complete the national picture alongside the MTCs at Aberdeen Royal Infirmary and Ninewells Hospital in Dundee opened in 2018, supporting all the component services within our Regional Networks.
It is to be hoped that by the time of next year’s report we will be able to reflect upon a time of challenge and change with a more secure feel for what the immediate and medium-term future holds for our service. This learning allows us to reenergise and reconvene with strength, determination and the confidence that comes from surmounting such a significant hurdle.
Every person and every collaborative and linked service involved, described and embraced within the following pages is deserving of the greatest of gratitude and recognition. We are indebted to you all.
The full report can be seen here.
Martin McKechnie
National Clinical Lead
Scottish Trauma Network
While there are fewer other activities to divert us and our children during this period, it’s great to see everyone getting out on their bikes. It’s such a great way to get out and about and good for our general health and wellbeing. Safety equipment, such as helmets, can be helpful to keep their heads safe in case of a tumble, especially for children who are a bit less stable on their bikes. Mark Lilley, one of the Major Trauma Co-ordinators in Glasgow put together this short video with some advice when we had some glorious weather during lockdown last Spring/Summer. Keep cycling!
Image credit: Creative Commons, Pressedienst Fahrrad
Executive Summary from Martin McKechnie
2019-20 was another significant and progressive year for the Scottish Trauma Network. There is much to champion, and more to come in what is shaping up to be an exciting 2020-21. That this has been achieved latterly against the backdrop of the Covid-19 pandemic, with the many necessary twists and turns in expectation, guidance, policy, redeployment and operational initiative across all our facets and collaborations within NHS Scotland, is yet further evidence of the energy, resilience and pragmatism shown by all members of our flourishing STN family.
By this time next year we expect to have delivered a fully operational STN, by opening our final Regional Major Trauma Centres at the Queen Elizabeth University Hospital in Glasgow, and at the Royal Infirmary in Edinburgh. This will complete the national picture alongside the MTCs at Aberdeen Royal Infirmary and Ninewells Hospital in Dundee, and support all the component services within our Regional Networks. To achieve this landmark against the turbulence of 2020 will indeed be cause for celebration.
The success of the Scottish Ambulance Service’s Trauma Desk, and its Covid-prompted transformation into a national Critical Care Desk, as well as that of ScotSTAR North operating from its new base at Aberdeen Airport, allows us to look at further developments in Red Team prehospital Critical Care delivery across Scotland.
‘The Trauma App’ collaboration between STN, the emergency department representatives from across the STN, EMQUIRE, daysix, the Digital Health & Care Institute and Innovate UK, continues to attract international interest as that project enters final development and simulation phases.
Our new Research and Innovation Group has begun its work to tell the story of the STN via data. As well as the R&I Group’s clinical research remit, there will be an assessment of the health and economic impact of the Scottish Government’s major investment in the STN.
In a new and exciting development to help tell this story, Firecrest Films, a Glasgow-based independent television production company, has been commissioned by Channel 4 to produce a flagship 6-part primetime documentary series on the work, patients and staff of the Scottish Trauma Network. It is hoped that filming will start in 2021.
Finally, as testament to the way the STN has developed and at the Cabinet Secretary for Health and Sport’s request, our model is being applied to support the development of several of the new Strategic Networks, where we are finding particular synergies with the Veterans and Health in Justice Networks.
Yet more interesting times ahead for the STN.
The STN Annual Report 2019/20 can be found HERE
Since its inaugural launch in February 2014 GESTS has developed a growing following and an international reputation.
This two-day symposium brings together a range of nationally and internationally renowned expertise and focuses on key messages and practical tips in emergency surgery and trauma care.
The event is designed to concentrate the most insightful updates into a highly focused and well-structured programme with opportunities to ask key questions. GESTS will not only consolidate your existing knowledge, but give you access to expert opinion, topical debate and key updates. Delegate feedback has repeatedly praised the informal nature of the meeting, the short, focused, talks, the case based panel discussions, and the range of speakers.
GESTS 2018 was the fastest selling event to date and we expect 2019 to sell out even faster
All the GESTS’ trademarks will be retained including short, exciting and clinically-relevant presentations, ample opportunity to challenge the faculty during open and lively discussion, practical advice to get you and your patient out of trouble and several lifetimes’ experience distilled down to key take home messages. We look forward to seeing you in Glasgow in February 2019!
For further details, download the full event flyer, and to book check out the GESTS website.